INTRODUCTION
In December 2019, Wuhan, China, had an outbreak of pneumonia of unknown cause. This led to a grave condition, in not only China but also globally.1 By January 7, 2020, Chinese scientists successfully isolated a novel coronavirus (nCoV) from patients in Wuhan. However, the rapid spread of this deadly virus forced World Health Organization (WHO) to declare COVID-19 or SARS-CoV-2 as a public health emergency of international concern (PHEIC).2 The coronavirus pandemic placed a burden on the healthcare system and affected healthcare services globally. It spread worldwide and created panic among everyone, nationally and internationally, as there was no cure for it during the initial times, and it spread quickly. There is a dire need to comprehend the effect of COVID-19 on various healthcare professionals in different parts of the country.
According to the Occupational Safety and Health Administration (OSHA) guidelines, dentists and dental workers are considered at high risk for the spread of COVID-19.3 The spread of viruses in a dental setting may be due to the distance that bioaerosols travel during dental management. The infectious microorganisms can spread through different courses like direct/indirect contact with salivary and nasopharyngeal drops from the affected patients, contact with debased instruments or dental water supply framework, and cross-pollutions from lifeless surfaces inside the dental settings.4 Health authorities have instructed the dental professionals to provide only emergency dental treatment for patients with suspected/confirmed COVID-19 subjects and to suspend routine procedures to control the spread of the COVID-19 infection. The role of dentists in preventing the spread of COVID-19 is therefore critically important. Dental assistants are focused on ensuring patient security and are also among the experts most in danger of any infectious disease, given the nearby contact with patients.
Dental colleges are important places for dental students, technicians, dental assistants, and faculty members to learn and grow together as a team, to provide the best treatment in routine dental practice to patients. With dental students, professors, and dental assistants, along with the patients, being involved in routine, the chances of being infected with COVID-19 are always present, and this needs further exploration. The COVID-19 pandemic has created chaos among the academia, particularly in healthcare, which has increased the levels of stress and anxiety.5 During this emergency, all the healthcare workers (HCWs), including medical caretakers, doctors, paramedical staff, and nursing and medical students, have been under a high level of stress and anxiety, both psychologically and physically.5,6,7,8
Even though most dental clinical settings were suspended in nations experiencing the COVID-19 pandemic, dental care experts are facing tremendous psychological pressure, knowing the reality of being in a higher-hazard group.9 While there are many studies10,11 in Saudi Arabia regarding stress levels, none concerned dental assistants who are equally exposed to COVID-19 as dentists. This research aims to assess the psychological impact of COVID-19 on dental assistants in Saudi Arabia during this pandemic.
MATERIALS AND METHODS
This questionnaire-based cross-sectional study was carried out from March 2022 to June 2022 after getting approval from the Institutional Review Board (IRB) at Riyadh Elm University, Saudi Arabia. The study included dental assistants working in various dental clinics and hospitals in Saudi Arabia. Other dental auxiliaries were excluded from this study. The psychological behavior of the dental assistants was assessed during the COVID-19 pandemic through a pre-validated Depression, Anxiety, Stress Scale with 21 Items (DASS-21) questionnaire.12 This survey consisted of two sections:
-
The first section included questions related to demographic details including age, gender, nationality, and marital status.
-
The second section included questions related to depression, anxiety, and stress. Each section consisted of seven items, related to depression, anxiety, and stress. The scoring was calculated on a four-point scale of “did not apply to me at all,” “applied to me to some degree,” “applied to me to a considerable degree,” and “applied to me very much.” The scores were calculated by adding the individual scores for the relevant items and interpreted as normal, mild, moderate, severe, and extremely severe as provided in Table 1.
TABLE 1. Scoring system for DASS-21 scale.
| Scoring | Depression | Anxiety | Stress |
|---|---|---|---|
| Normal | 0–4 | 0–3 | 0–7 |
| Mild | 5–6 | 4–5 | 8–9 |
| Moderate | 7–10 | 6–7 | 10–12 |
| Severe | 11–13 | 8–9 | 13–16 |
| Extremely Severe | 14+ | 10+ | 17+ |
Data (emails) from dental assistants were obtained from the dental assistant society. A total of 280 questionnaires were sent to the dental assistants via email using Google Forms. One reminder email was sent after a week to fill out and submit the form. The completed questionnaire was considered as their consent to participate in the study. No information revealed the identity of the study participants.
Statistical Analysis
Data were tabulated in Microsoft Office Excel 2019, and the analysis was performed using Statistical Package for the Social Sciences (SPSS) (IBM, New York City, USA) Version 23.0. Descriptive statistical measures were employed to summarize the data.
RESULTS
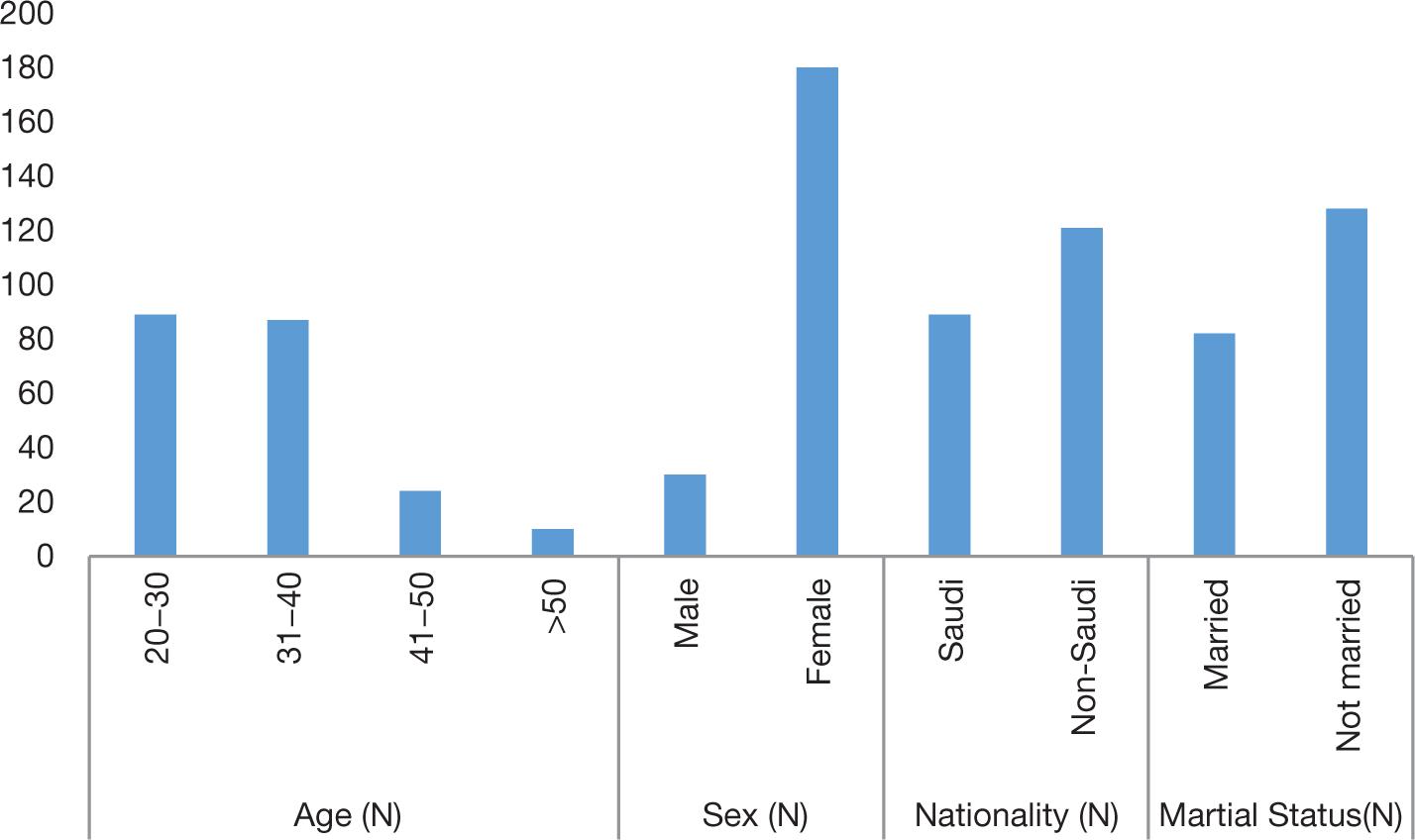
The response rate was 75% (210 out of 280). Figure 1 depicts the demographics of the study subjects. Most assistants were 20–40 years old and only 10 were above 50 years of age. Most participants were females (180) and were of non-Saudi origin.
FIG 1. Demographic characteristics of the study sample.
Response to the depression questions
Tables 2, 3, and 4 display the response of the study participants to the questions on the DASS questionnaire. Of the participants, 49.04% did not experience any positive feeling to some degree and 41.42% of the dental assistants found it challenging to work during the pandemic to some degree. Out of 210 participants, 117 did not feel that they did not have anything to look forward to. In the fourth question related to depression, 41.43% of subjects felt downhearted and blue to some degree during the COVID pandemic. Only 10 participants could not become enthusiastic about anything; but this was true for 42.38% of subjects to some degree. Eight subjects chose the “Applied to me very much” option for the question, “During the COVID-19 pandemic period, I felt I was not worth much as a person.” Around 62 people felt that life was meaningless during the COVID-19 pandemic.
TABLE 2. Response of DASS questionnaire (Depression) by the study participants (n = 210).
| Question | Options | N | Percentage |
|---|---|---|---|
| DEPRESSION—SEVEN ITEMS | |||
| 1. During the COVID-19 pandemic period, I could not seem to experience any positive feeling at all | Applied to me to a considerable degree | 30 | 14.29 |
| Applied to me to some degree | 103 | 49.04 | |
| Applied to me very much | 13 | 6.19 | |
| Did not apply to me at all | 64 | 30.48 | |
| 2.During the COVID-19 pandemic period, I found it difficult to work up the initiative to do things | Applied to me to a considerable degree | 34 | 16.20 |
| Applied to me to some degree | 87 | 41.42 | |
| Applied to me very much | 16 | 7.61 | |
| Did not apply to me at all | 73 | 34.76 | |
| 3.During the COVID-19 pandemic period, I felt that I had nothing to look forward to | Applied to me to a considerable degree | 15 | 7.14 |
| Applied to me to some degree | 70 | 33.33 | |
| Applied to me very much | 8 | 3.81 | |
| Did not apply to me at all | 117 | 55.71 | |
| 4.During the COVID-19 pandemic period, I felt downhearted and blue | Applied to me to a considerable degree | 33 | 15.71 |
| Applied to me to some degree | 87 | 41.43 | |
| Applied to me very much | 14 | 6.67 | |
| Did not apply to me at all | 76 | 36.19 | |
| 5.During the COVID-19 pandemic period, I was unable to become enthusiastic about anything | Applied to me to a considerable degree | 27 | 12.86 |
| Applied to me to some degree | 89 | 42.38 | |
| Applied to me very much | 10 | 4.76 | |
| Did not apply to me at all | 84 | 40 | |
| 6.During the COVID-19 pandemic period, I felt I was not worth much as a person | Applied to me to a considerable degree | 13 | 6.19 |
| Applied to me to some degree | 42 | 20 | |
| Applied to me very much | 8 | 3.81 | |
| Did not apply to me at all | 147 | 70 | |
| 7.During the COVID-19 pandemic period, I felt that life was meaningless | Applied to me to a considerable degree | 12 | 5.71 |
| Applied to me to some degree | 41 | 19.52 | |
| Applied to me very much | 9 | 4.29 | |
| Did not apply to me at all | 148 | 70.48 | |
TABLE 3. Response of DASS questionnaire (Anxiety) by the study participants (n = 210).
| Question | Options | N | Percentage |
|---|---|---|---|
| ANXIETY—SEVEN ITEMS | |||
| 1.During the COVID-19 pandemic period, I was aware of dryness of my mouth | Applied to me to a considerable degree | 25 | 11.91 |
| Applied to me to some degree | 66 | 31.42 | |
| Applied to me very much | 14 | 6.67 | |
| Did not apply to me at all | 105 | 50 | |
| 2.During the COVID-19 pandemic period, I experienced breathing difficulty (e.g., excessively rapid breathing, breathlessness in the absence of physical exertion) | Applied to me to a considerable degree | 14 | 6.67 |
| Applied to me to some degree | 42 | 20 | |
| Applied to me very much | 8 | 3.81 | |
| Did not apply to me at all | 146 | 69.52 | |
| 3.During the COVID-19 pandemic period, I experienced trembling (e.g., in the hands) | Applied to me to a considerable degree | 10 | 4.76 |
| Applied to me to some degree | 34 | 16.19 | |
| Applied to me very much | 9 | 4.29 | |
| Did not apply to me at all | 157 | 74.76 | |
| 4.During the COVID-19 pandemic period, I was worried about situations in which I might panic and make a fool of myself | Applied to me to a considerable degree | 12 | 5.71 |
| Applied to me to some degree | 75 | 35.71 | |
| Applied to me very much | 14 | 6.67 | |
| Did not apply to me at all | 109 | 51.90 | |
| 5.During the COVID-19 pandemic period, I felt I was close to panic | Applied to me to a considerable degree | 12 | 5.71 |
| Applied to me to some degree | 66 | 31.43 | |
| Applied to me very much | 14 | 6.67 | |
| Did not apply to me at all | 118 | 56.19 | |
| 6.During the COVID-19 pandemic period, I was aware of the action of my heart in the absence of physical exertion (e.g., sense of heart rate increase, heart missing a beat) | Applied to me to a considerable degree | 15 | 7.14 |
| Applied to me to some degree | 51 | 24.28 | |
| Applied to me very much | 13 | 6.19 | |
| Did not apply to me at all | 131 | 62.38 | |
| 7.During the COVID-19 pandemic period, I felt scared without any good reason | Applied to me to a considerable degree | 19 | 9.04 |
| Applied to me to some degree | 79 | 37.61 | |
| Applied to me very much | 13 | 6.19 | |
| Did not apply to me at all | 99 | 47.14 | |
TABLE 4. Response of DASS questionnaire (Stress) by the study participants (n = 210).
| Question | Options | N | Percentage |
|---|---|---|---|
| STRESS—SEVEN ITEMS | |||
| 1.During the COVID-19 pandemic period, I found it hard to wind down (relax) | Applied to me to a considerable degree | 19 | 9.05 |
| Applied to me to some degree | 81 | 38.57 | |
| Applied to me very much | 13 | 6.19 | |
| Did not apply to me at all | 97 | 46.19 | |
| 2.During the COVID-19 pandemic period, I tended to overreact to situations | Applied to me to a considerable degree | 18 | 8.57 |
| Applied to me to some degree | 95 | 45.24 | |
| Applied to me very much | 12 | 5.71 | |
| Did not apply to me at all | 85 | 40.47 | |
| 3.During the COVID-19 pandemic period, I felt that I was using a lot of nervous energy | Applied to me to a considerable degree | 12 | 5.71 |
| Applied to me to some degree | 72 | 34.29 | |
| Applied to me very much | 16 | 7.62 | |
| Did not apply to me at all | 110 | 52.38 | |
| 4.During the COVID-19 pandemic period, I found myself getting agitated (upset) | Applied to me to a considerable degree | 30 | 14.29 |
| Applied to me to some degree | 89 | 42.38 | |
| Applied to me very much | 7 | 3.33 | |
| Did not apply to me at all | 84 | 40 | |
| 5.During the COVID-19 pandemic period, I found it difficult to relax | Applied to me to a considerable degree | 23 | 10.95 |
| Applied to me to some degree | 83 | 39.52 | |
| Applied to me very much | 9 | 4.28 | |
| Did not apply to me at all | 95 | 45.24 | |
| 6.During the COVID-19 pandemic period, I was intolerant of anything that kept me from getting on with what I was doing | Applied to me to a considerable degree | 21 | 10 |
| Applied to me to some degree | 79 | 37.62 | |
| Applied to me very much | 7 | 3.33 | |
| Did not apply to me at all | 103 | 49.05 | |
| 7.During the COVID-19 pandemic period, I felt that I was rather touchy (oversensitive) | Applied to me to a considerable degree | 28 | 13.33 |
| Applied to me to some degree | 84 | 40 | |
| Applied to me very much | 8 | 3.81 | |
| Did not apply to me at all | 90 | 42.86 | |
Response to the anxiety questions
Most subjects (69.52%) did not experience breathing difficulty (e.g., excessively rapid breathing, breathlessness in the absence of physical exertion) during the COVID-19 pandemic. Only nine (“Applied to me very much” category) subjects experienced trembling in their hands. Less than half of the subjects were worried about situations in which they might panic and make a fool of themselves during the pandemic. Around 111 dental assistants felt scared without any good reason.
Response to the stress questions
Most assistants (113, 53.8%) managed to relax during the COVID-19 pandemic with varying severity. Of the subjects, 45.24% chose (“Applied to me to some degree” category) on questions about overreacting to a situation and 52.38% did not feel nervous during the COVID-19 pandemic. Around 120 subjects felt oversensitive during the pandemic period (Tables 2, 3, and 4).
Depression score was more in the age group of 20–30 years (5.281), which was slightly lower than in the age group of 41–50 (5.29) years and above 50 years (6.00) and more than the age group of 31–40 years. The comparison was statistically nonsignificant. Anxiety score was highest among 20–30 years old (4.978) and minimum in the age group of 41–50 years (2.83) and the difference was not statistically significant. Similarly, the stress scores among the different age groups were not statistically significant (p = 0.731). The details are summarized in Table 5.
TABLE 5. Comparison of DASS scores based on age groups.
| N | Mean | SD | Standard Error | 95% Confidence Interval for Mean | Minimum | Maximum | p | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||||||
| Depression | 20–30 | 89 | 5.281 | 4.5352 | 0.4807 | 4.326 | 6.236 | 0 | 18.0 | 0.845 |
| 31–40 | 87 | 4.874 | 4.5233 | 0.4850 | 3.910 | 5.838 | 0 | 21.0 | ||
| 41–50 | 24 | 5.292 | 3.1962 | 0.6524 | 3.942 | 6.641 | 0 | 13.0 | ||
| Above 50 | 10 | 6.000 | 4.5216 | 1.4298 | 2.765 | 9.235 | 0 | 15.0 | ||
| Total | 210 | 5.148 | 4.3772 | 0.3021 | 4.552 | 5.743 | 0 | 21.0 | ||
| Anxiety | 20–30 | 89 | 4.978 | 5.0811 | 0.5386 | 3.907 | 6.048 | 0 | 21.0 | 0.150 |
| 31–40 | 87 | 3.793 | 4.4958 | 0.4820 | 2.835 | 4.751 | 0 | 21.0 | ||
| 41–50 | 24 | 2.833 | 3.5098 | 0.7164 | 1.351 | 4.315 | 0 | 16.0 | ||
| Above 50 | 10 | 4.100 | 2.2336 | 0.7063 | 2.502 | 5.698 | 0 | 7.0 | ||
| Total | 210 | 4.200 | 4.6151 | 0.3185 | 3.572 | 4.828 | 0 | 21.0 | ||
| Stress | 20–30 | 89 | 5.494 | 4.8760 | 0.5169 | 4.467 | 6.522 | 0 | 19.0 | 0.731 |
| 31–40 | 87 | 5.195 | 5.0528 | 0.5417 | 4.118 | 6.272 | 0 | 21.0 | ||
| 41–50 | 24 | 4.292 | 3.3164 | 0.6769 | 2.891 | 5.692 | 0 | 14.0 | ||
| Above 50 | 10 | 5.700 | 4.3982 | 1.3908 | 2.554 | 8.846 | 0 | 16.0 | ||
| Total | 210 | 5.243 | 4.7646 | 0.3288 | 4.595 | 5.891 | 0 | 21.0 | ||
| Total score | 20–30 | 89 | 15.75 | 13.285 | 1.408 | 12.95 | 18.55 | 0 | 56 | 0.613 |
| 31–40 | 87 | 13.86 | 13.301 | 1.426 | 11.03 | 16.70 | 0 | 63 | ||
| 41–50 | 24 | 12.42 | 8.787 | 1.794 | 8.71 | 16.13 | 1 | 43 | ||
| Above 50 | 10 | 15.80 | 10.401 | 3.289 | 8.36 | 23.24 | 0 | 38 | ||
| Total | 210 | 14.59 | 12.715 | 0.877 | 12.86 | 16.32 | 0 | 63 | ||
SD, standard deviation.
The results were statistically significant (p = 0.001) in the comparison of the DASS scores between males and females. The mean total DASS score was higher in males (20.03) compared to females (13.68) as summarized in Table 6.
The scores for depression (5.966), anxiety (5.494), and stress (6.034) were more in Saudi-origin dental assistants when compared to non-Saudi subjects and the results were also statistically significant as mentioned in Table 7.
TABLE 6. Comparison of DASS scores based on gender.
| Sex | N | Mean | SD | Standard Error Mean | p | |
|---|---|---|---|---|---|---|
| Depression | Male | 30 | 5.933 | 5.6198 | 1.0260 | 0.019* |
| Female | 180 | 5.017 | 4.1393 | 0.3085 | ||
| Anxiety | Male | 30 | 6.833 | 6.5447 | 1.1949 | 0.001* |
| Female | 180 | 3.761 | 4.0711 | 0.3034 | ||
| Stress | Male | 30 | 7.267 | 6.0226 | 1.0996 | 0.011* |
| Female | 180 | 4.906 | 4.4530 | 0.3319 | ||
| Total score | Male | 30 | 20.03 | 17.139 | 3.129 | 0.001* |
| Female | 180 | 13.68 | 11.635 | 0.867 |
*Denotes significant values. SD, standard deviation.
TABLE 7. Comparison of DASS scores based on nationality.
| Nationality | N | Mean | SD | Standard Error Mean | p | |
|---|---|---|---|---|---|---|
| Depression | Saudi | 89 | 5.966 | 4.9416 | 0.5238 | 0.004* |
| Non-Saudi | 121 | 4.545 | 3.8210 | 0.3474 | ||
| Anxiety | Saudi | 89 | 5.494 | 5.4212 | 0.5746 | 0.000* |
| Non-Saudi | 121 | 3.248 | 3.6590 | 0.3326 | ||
| Stress | Saudi | 89 | 6.034 | 5.3692 | 0.5691 | 0.016* |
| Non-Saudi | 121 | 4.661 | 4.1943 | 0.3813 | ||
| Total score | Saudi | 89 | 17.49 | 14.595 | 1.547 | 0.001* |
| Non-Saudi | 121 | 12.45 | 10.701 | 0.973 |
*Denotes significant values. SD, standard deviation.
As shown in Table 8, there was no statistical difference in total and individual DASS scores between married and unmarried dental assistants.
TABLE 8. Comparison of DASS scores based on marital status.
| Marital Status | N | Mean | SD | Standard Error Mean | p | |
|---|---|---|---|---|---|---|
| Depression | Married | 82 | 5.183 | 4.5600 | 0.5036 | 0.534 |
| Not married | 128 | 5.125 | 4.2741 | 0.3778 | ||
| Anxiety | Married | 82 | 3.927 | 4.7682 | 0.5266 | 0.738 |
| Not married | 128 | 4.375 | 4.5246 | 0.3999 | ||
| Stress | Married | 82 | 5.537 | 5.1333 | 0.5669 | 0.652 |
| Not married | 128 | 5.055 | 4.5234 | 0.3998 | ||
| Total score | Married | 82 | 14.65 | 13.539 | 1.495 | 0.926 |
| Not married | 128 | 14.55 | 12.212 | 1.079 |
SD, standard deviation.
DISCUSSION
Dentistry involves close contact with patients, which can lead to the transmission of the coronavirus to the dentist and the other dental staff. The people infected with the coronavirus may not show symptoms during the initial stages of infection, making them a possible source of virus transmission to the dental HCWs (dentists and assistants) while seeking treatment. As a result, dentists and their assistants are at risk of contamination while carrying out routine dental procedures.13 The current guidelines on the COVID-19 outbreak recommend delaying all nonemergency dental treatment, and only patients with acute pain, swelling, or trauma are advised to visit a dentist.14 The COVID-19 pandemic has caused a lot of psychological pressure on HCWs, which has affected the health of HCWs, such as doctors, nurses, and dentists. This study focused on the psychological impact of COVID-19 on dental assistants in Saudi Arabia.
The concern raised here is about the dental assistants because of their crucial position in the smooth running of the dental clinic. They communicate with potentially infected patients and encounter patients’ noncompliance with hygiene instructions in the waiting area. Another factor contributing to stress is inadequate staffing during the COVID-19 pandemic.15,16 The DASS-21 questionnaire, a shorter version of the elaborated DASS-41, is often used in research17,18 related to mental health and practices. With the overall and individual subscales of Cronbach’s alpha (0.96) showing exceptional internal consistency for the DASS-21 instrument, this questionnaire was used in this study.19
A total of 210 dental assistants participated and completed the online DASS questionnaire, displaying a substantial study sample size. The socio--demographic data represent more female dental assistants participating in the survey than males, similar to the other study from Saudi by Ali et al.20 Most participants were in the age group of 20–40 years, similar to the discussed regular age and corresponding employment features in various studies in Germany and Saudi Arabia.20,21
The depression, anxiety, and stress scores were higher in males than females, with statistically significant differences. This could be due to fear in male participants of this survey and the low numbers of males employed in this profession. Similar results were obtained in previous studies where female participants did not show higher psychological stress scores than male colleagues.22,23,24 Marital status did not significantly affect the DASS scores. Parents and family members provide moral support for various problems, which boosts a person positively and gives strength to overcome mental distress.25,26 However, in other studies, subjects with no relationships displayed more sound mental health than the married participants, especially those with poor relationship quality.27
Depressive conditions, anxiety, and stress at the workplace are the most prominent reasons for mental problems worldwide. Previous literature showed that dentists and other HCWs face occupational stressors, such as the risk of infection, continuous pressure, anxiety about their capability to deliver satisfactory health services in the future, and financial burdens.28,29,30 These factors have aggravated anxiety among dental professionals all over the country during the COVID-19 pandemic. Pandemics bring about psychological consequences, such as fear and anxiety, mainly when the number of infected people and the mortality ratio are high.31 According to a study, around one-third of dental assistants preferred emergency dental treatment alone and reported significantly more anxiety regarding COVID-19 infection transmission than other groups (p < 0.05).32 Most dental practitioners feared contracting COVID infection from a patient, which was significantly related to high levels of psychological distress.33,34 Nurses (closest similarity to dental assistants) have reported increased pain levels than other frontline HCWs,35,36,37,38,39 while some studies reported no difference in the stress levels.39,40
Only one study highlighted a higher rate of stress in doctors.41 Dental health professionals are a significant part of the healthcare system.42 The adverse effect of COVID-19 on their mental health (psychological impact) must not be ignored, and preventive measures must be considered. Training and education regarding COVID-19 guidelines for controlling the transmission of the infection, followed by the execution of these measures for a safe working setting, will create room for the optimistic psychological minds of dental professionals treating patients during emergency times.
LIMITATIONS
First, this is a cross-sectional study so no -follow-up could be performed. Further, the voluntary option to be part of this study must have led to a selection bias.
CONCLUSION
Frontline HCWs in direct contact with COVID-19 patients had higher distress symptoms. There was a significant difference in DASS scores in both gender and the origin of dental assistants. It is essential for the governments to be concerned about the mental health of the HCWs to avoid adverse psychological impacts on their health. The guidelines and restrictions measures implemented by different countries might also affect the practice and mental health of HCWs.