INTRODUCTION
The Problast implant (Allow plastic) is a new modified material,1 designed especially for cosmetic restoration. It is ultra-porous (70–90% porous by volume) and painted with a mixture2 of biocompatible materials to promote the bone growth. The porous Problast implant has been used in this new technique as a sub-periosteal implant to restore the missing part of the Zygomatic bone in a facial trauma.3 It is also used among patients who are contraindicated to bone graft or refuse such surgery. It is an option when the surgery fails, owing to insufficient blood supply in the recipient area or excessive scar tissue that provides insufficient tissue to cover the bone transplant without tension.
MATERIALS AND METHOD
The ultra-porous Problast implant is painted (in some cases immersed totally) with a mixture of a biocompatible phosphate containing oily calcium suspension,4 which (stimulate the osteo conduction) in combination with a porous Hydroxyl apatite, promote bone formation through the porous Problast implant. All of these materials are biocompatible (inert), which means that they are not rejected by patient tissues.
SURGICAL TECHNIQUE
To prepare the patients for surgery, a complete medical history as well as the mode of onset, and the duration of the injury are recorded, hematological examination, and x-rays of the face (lateral oblique, true lateral, and posterior anterior views) are profound.
In the operating room, an autoclaved Problast is scrapple to the required shape to give it a good aesthetic aspect. The carved Problast is inserted through the coronal incision if a ready-made shaped Problast is found (Figures 1 and 2) by an extra oral approach.
FIGURE 1. Ready-made shaped Problast.
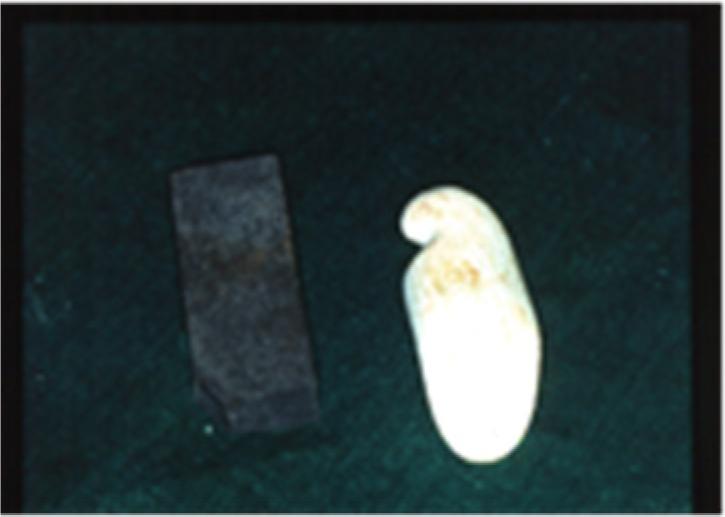
FIGURE 2. The Problast carved by scrapple.

Under a general anesthesia, with oro endo tracheal intubation, a dissection through a coronal incision is carried down from the lateral orbital rim to the lower border of the zygoma, just inferior to the orbital rim, angulated below the inferior orbital nerve close to the pyriform aperture medially, and just above the upper sulcus inferiorly, to create enough space to accumulate the subperiosteal implant. It is not necessary to fix the subperiosteal Problast implant to the underlining bones as in a bone graft. The ingrowth of fibrous tissues through the porosities of the subperiosteal implant give it a good temporary fixation. The wound is then sutured in layers without tension to avoid resorption of the implant by the pressure (since the Problast implant has a low crushing strength).
POST-OPERATIVE
The patient is instructed to avoid sleeping on the operated side for few weeks to avoid any resorption of the implant. It is not necessary to prescribe any antibiotic as prophylaxis cover. The Alloplastic Problast is a radiolucent material. Thus, a regular post-operative/clinical follow up study for a period of three years is needed, until clear a bone deposition seen in the X-ray.
RESULT AND CONCLUSION
The patients with bullet injuries were found to have a non-satisfactory result due to the comminuted5,6 fracture of the zygoma, super imposed by an infection.7 The bone spicules start to in grow in the sub-periosteal implant in about eight weeks (Table 1). No clinical difference was found between the painted Problast implant and the totally immersed problast in the mixture of compatible materials.8-10 In 3–5 years, all the Problast implant is expected to be resorped and replaced by bone, followed by a remodeling of the bone. This gives a natural aesthetic appearance to the zygomatic bone, which means that the Problast implant has transformed to a normal living bone.11 This innovative and new surgical technique is in need of more research, and constant follow-up is necessary to observe the deposition of bone and the final permanent aesthetic appearance. This new surgical technique is a relatively easy, simple, non-traumatic surgery, with less time consumed by the surgeon in the operating theater, delivering a satisfactory final aesthetic aspect.
TABLE 1. Demographic data of patients with different type of trauma treated by a sub-periosteal implant mixed with a biocompatible material
| No. of patients | Age | Sex | Type of trauma | Result |
|---|---|---|---|---|
| 3 | 25–30 | Male | Traffic Accident | Satisfactory |
| 1 | 28 | Male | Shell Injury | Satisfactory |
| 2 | 30–36 | Male | Bullet Injury | Non Satisfactory |