INTRODUCTION
Coronavirus disease was established as a global pandemic by the World Health Organization (WHO) on 11th of march 2020.1,2 The causative agent, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is a new virus that is primarily transmitted by direct or indirect personal contact via airborne respiratory droplets from an infected person.3 To restrict the spread of this pandemic, governments of various countries have ingrained policies such as face masks, maintenance of social distancing, measures to curb business operations, people’s transit, and cancellation of reservations, services, social gatherings, and events.2,4 Due to these restraints and lockdown periods, people were compelled to stay at home, resulting in job loss and rise in insecurities, fears, and concerns, ultimately decreasing the quality of life globally.5
Although the medical perception suggests that children are not at an increased risk of infection by the coronavirus disease 2019 (COVID-19), this pandemic has crucially impacted the lives of children.6 Closure of schools and sports activities during this global pandemic situation has forced children to stay at home which has engendered alteration in their routine activities affecting them physically as well as psychologically.7,8 Individuals who are overblown by COVID-19 are also at a greater risk for oral diseases and might experience oral healthcare-related discrepancies at a higher rate.9 On the other hand, the COVID-19 pandemic has resulted in reduced working hours for dental practitioners except for emergency services, thus limiting routine dental care and prevention provided to the patients.10 The present study was undertaken to analyze the impact of the coronavirus pandemic on children’s oral health and caregivers’ attitudes towards teledentistry in AlJahra city, Kuwait.
MATERIAL AND METHODS
Ethical Clearance
The questionnaire used in the present study was formulated by the Department of Preventive Dentistry. The questionnaire was anonymous to ensure privacy protection. Ethical approval for the study was obtained and the proposal was registered with the research center of the Ministry of Health in Kuwait. Informed consent was obtained from each participant.
Study Sample and Data collection
An electronic self-structured questionnaire was created using a Google survey (www.google.survey.com) distributed to 583 caregivers of children aged between 3 and 10 years in AlJahra city, Kuwait using the caregiver’s via electronic messages.
Questionnaire Survey
The questionnaire consisted of nine multiple choice questions divided equally into three parts. The first part included demographic data questions, including age, gender, and educational level of the caregivers. For ease of understanding, the age range was divided into three groups 20–30 years, 30–40 years, and more than 40 years. The second part addressed the assessment of the oral health status of the children by their caregivers during the lockdown, the influence of pandemics on the oral health of children, and the reasons for the same. The third part was related to the caregiver’s attitude towards the healthcare system and teledentistry.
Validation of questionnaire
A self-structured questionnaire was designed using the Arabic language. A pilot study was done on 20 participants to assess the questioner’s inter-rater validity using subject experts and agreement analysis. The kappa score for an agreement was 0.89.
Statistical analysis
The number of subjects and percentages were reported for categorical data. The bar charts and clustered bar charts were displayed for categorical data. The Pearson’s Chi-square test and Fisher’s Exact test (less cell count) were used to assessing the association between categorical variables. All analyses were done using Statistical Package for Social Sciences (SPSS) software Version 21.0 (Armonk, NY: IBM Corp).
RESULTS
In the present study, out of 583 participants from AlJahra city, Kuwait 60% were in the age group of 30–40 years, 27.6% were in the age group of 20–30 years, and 12.4% were more than 40 years of age. Forty-four percent were male, whereas 56% were females. Regarding educational level, 62.3% of the participants were graduates, 22.1% had master’s degrees, and 15.6% were high school pass out or similar (Table 1). Around 93.5% of the participants were not satisfied with their child’s oral health status, out of which 256 were male and 289 were female (Table 2). Also, most of the participants who were not satisfied with their child’s oral health were aged 30–40 years (Table 3) and were graduates (Table 4). However, the remaining 6.5% of the participants who were satisfied with child’s oral health status were female (p <0.001) (Table 3). Two hundred and seventy one participants agreed that the pandemic had a negative effect on their child’s oral health status, 262 agreed to some extent. At the same time, 50 of them disagree that the pandemic had a negative impact on their child’s oral health status (Table 2).
TABLE 1. Demographic characteristics of the study participants.
| Characteristics | n (%) |
|---|---|
| Age (years) 20–30 30–40 >40 |
161 (27.6) 350 (60.0) 72 (12.4) |
| Gender Male Female |
256 (43.9) 327 (56.1) |
| Educational level High school or associate Bachelor Graduate degree (Masters’, PhD) |
91 (15.6) 363 (62.3) 129 (22.1) |
TABLE 2. Association of study variables based on gender.
| Question | Total n (%) |
Male n (%) |
Female n (%) |
P value |
|---|---|---|---|---|
| Are you satisfied with your children’s oral health status? Yes No |
38 (6.5) 545 (93.5) |
0 (0.0) 256 (100.0) |
38 (6.5) 289 (88.4) |
<0.001 |
| Does the pandemic negatively affect your child’s oral status? Agree to some extent Totally agree Disagree |
262 (44.9) 271 (46.5) 50 (8.6) |
134 (52.3) 96 (37.5) 26 (10.2) |
128 (39.1) 175 (53.5) 24 (7.3) |
0.001 |
| In your opinion, can healthcare be provided via teledentistry (technology) to solve your children’s oral health problem? Agree to some extent Totally agree Don’t Know Disagree |
232 (39.8) 1 (0.2) 310 (53.2) 40 (6.9) |
74 (28.9) 0 (0.0) 145 (56.6) 37 (14.5) |
158 (48.3) 1 (0.3) 165 (50.5) 3 (0.9) |
<0.001 |
| Do you use teledentistry services during the pandemic? Yes No |
544 (93.3) 39 (6.7) |
254 (99.2) 2 (0.8) |
290 (88.7) 37 (11.3) |
<0.001 |
TABLE 3. Association of study variables based age group of study participants
| Question | Total n (%) |
>20-30 years n (%) |
30-40 years n (%) |
>40 years n (%) |
P value |
|---|---|---|---|---|---|
| Are you satisfied with your children’s oral health status? Yes No |
38 (6.5) 545 (93.5) |
13 (8.1) 148 (91.9) |
24 (6.9) 326 (93.1) |
1 (1.4) 71 (98.6) |
0.133 |
| Does the pandemic negatively affect your child’s oral status? Agree to some extent Totally agree Disagree |
262 (44.9) 271 (46.5) 50 (8.6) |
71 (44.1) 59 (36.6) 31 (19.3) |
170 (48.6) 161 (46.0) 19 (5.4) |
21 (29.2) 51 (70.8) 0 (0.0) |
<0.001 |
| In your opinion, can healthcare be provided via teledentistry (technology) to solve your children’s oral health problems? Agree to some extent Totally agree Don’t Know Disagree |
232 (39.8) 1 (0.2) 310 (53.2) 40 (6.9) |
56 (34.8) 0 (0.0) 92 (57.1) 13 (8.1) |
138 (39.4) 0 (0.0) 205 (58.6) 7 (2.0) |
38 (52.8) 1 (1.4) 13 (18.1) 20 (27.8) |
<0.001 |
| Do you use teledentistry services during the pandemic? Yes No |
544 (93.3) 39 (6.7) |
149 (92.5) 12 (7.5) |
324 (92.6) 26 (7.4) |
71 (98.6) 1 (1.4) |
0.139 |
TABLE 4. Association of study variables based on the qualification of study participants
| Question | Total n(%) |
High school n(%) |
Bachelors n(%) |
Masters/ PhD n(%) |
P value |
|---|---|---|---|---|---|
| Are you satisfied with your children’s oral health status? Yes No |
38 (6.5) 545 (93.5) |
13 (4.3) 78 (85.7) |
24 (6.6) 339 (93.4) |
1 (0.8) 128 (99.2) |
<0.001 |
| Does the pandemic negatively affect your child’s oral status? Agree to some extent Totally agree Disagree |
262 (44.9) 271 (46.5) 50 (8.6) |
47 (51.6) 34 (37.4) 10 (11.0) |
152 (41.9) 184 (50.7) 27 (7.4) |
63 (48.8) 53 (41.1) 13 (10.1) |
0.115 |
| In your opinion, can healthcare be provided via teledentistry (technology) to solve your children’s oral health problem? Agree to some extent Totally agree Don’t Know Disagree |
232 (39.8) 1 (0.2) 310 (53.2) 40 (6.9) |
19 (20.9) 1 (1.1) 70 (76.9) 1 (1.1) |
171 (47.1) 0 (0.0) 177 (48.8) 15 (4.1) |
42 (32.6) 0 (0.0) 63 (48.8) 24 (18.6) |
<0.001 |
| Do you use teledentistry services during the pandemic? Yes No |
544 (93.3) 39 (6.7) |
79 (86.8) 12 (13.2) |
338 (93.1) 25 (6.5) |
127 (98.4) 2 (1.6) |
0.002 |
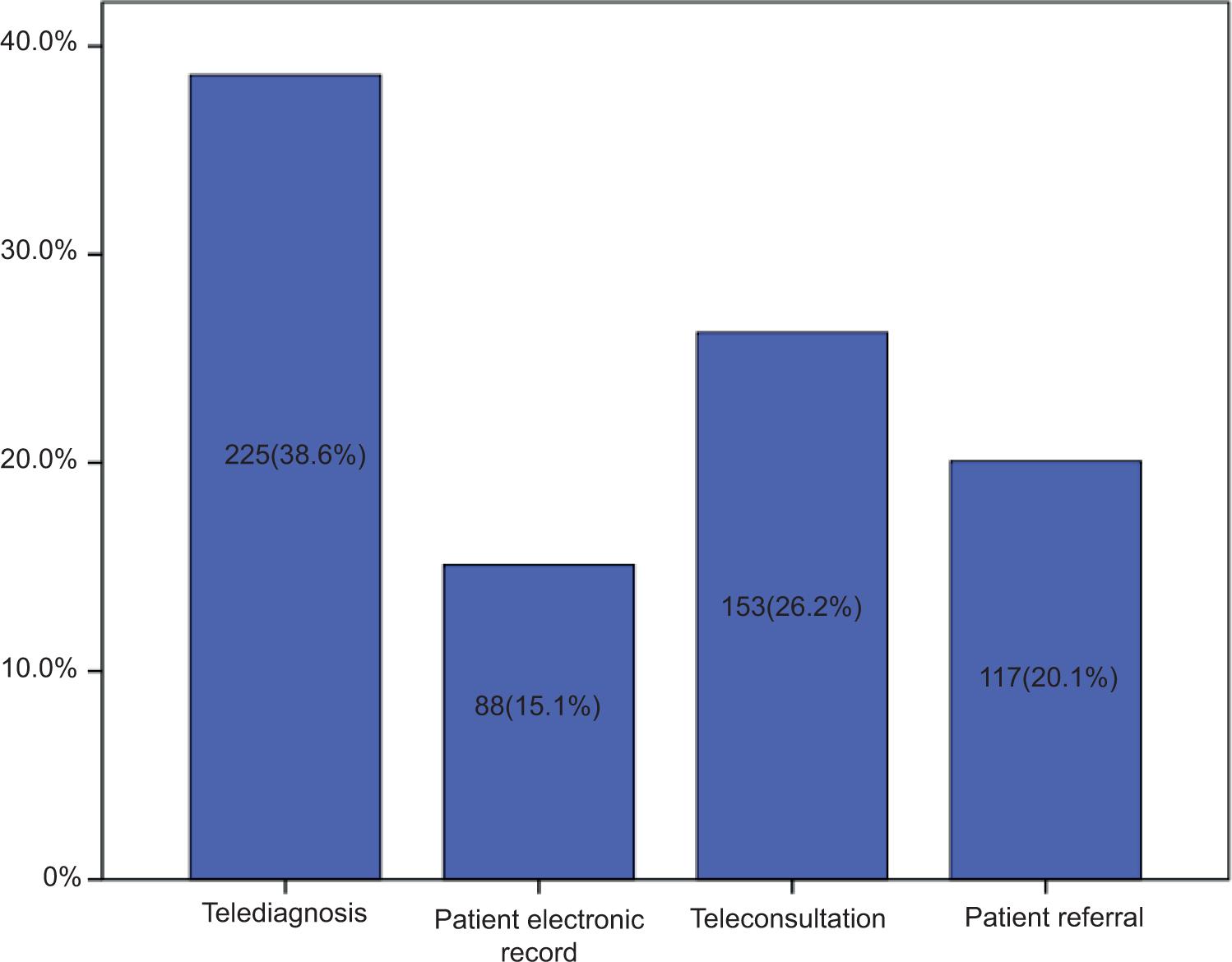
According to the participants, the most common reason that affected their child’s oral health status during the pandemic was the change in sleep pattern (34.3%), followed by feeding style (32.8%) and quarantine and social restriction (32.9%) (Figure 1). Around 53.2% of the participants did not know if teledentistry could be used to meet their children’s oral healthcare needs. Approximately 39.8% of the participants agreed that oral healthcare can be provided through teledentistry for their children, out of which 74 were male and 158 were female (p<0.001). However, merely 0.2% of participants agreed that teledentistry could be useful to meet the oral healthcare needs of their children during pandemics, while 6.7% disagreed (Table 2). During the pandemic, 93.3% of the participants have utilized teledentistry services, out of which 254 were male and 290 were female (p<0.001) (Table 4). Around 38.6% of the participants think teledentistry can be most effectively used for telediagnosis, while 26.2% think it can be most beneficial for teleconsultation. Twenty percent believed that patient referral is the most common aspect of teledentistry used for children, and 15.1% believed that maintenance of a patient’s electronic record is the most effective health service provided by teledentistry (Figure 2).
FIGURE 1. Responses of caregivers regarding reason that affected their child’s oral health during pandemic period.
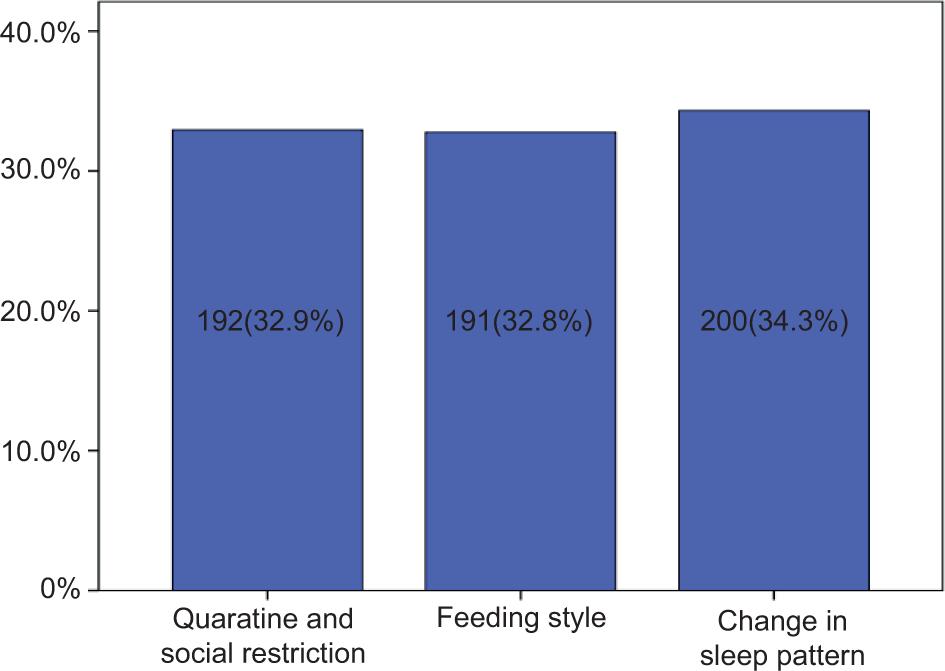
FIGURE 2. Responses of caregivers regarding the most useful aspect of teledentistry in dental appointments.
DISCUSSION
Oral health plays a vital role in the overall general health and social well-being of an individual. The mouth is crucial for smiling, speaking, eating, and quality of life. Dental caries and periodontal diseases are the most common conditions affecting the oral cavity, which are highly avertible.10,11 Populations that are at risk for chronic diseases are most likely to be at a higher risk for developing oral diseases. COVID-19 pandemic has led to a rise in stress levels, alcohol, and tobacco use, unhealthy and poor dietary intake, domestic violence, behavioral issues, and poverty. All these are common risk factors for the development and exacerbation of chronic diseases and poor oral health conditions.9
COVID-19-associated stress factors like a sudden increase in encounters with illness and demise of closed ones, closure of schools and sports activities, longer periods of at-home stay, restriction on peoples’ movements and social gatherings have detrimental effects on children’s psychological health.12–14 In addition to this, access to general and mental health resources has also been hindered in an attempt to decrease community transmission of COVID-19 disease.13–15 Tali et al.16 in their survey study found that exposure to stress during the COVID-19 pandemic was associated with worsening psychological well-being of youth. A similar study from Pakistan suggested a high prevalence of poor psychological well-being (41.2%) among the general population during the COVID-19 pandemic situation.17 Research indicates a strong correlation between psychological components like stress, depression, anxiety, and loneliness and oral conditions such as caries, erosion, and periodontal disease.18 Thus, with the increase in the COVID-19 pandemic’s impact on mental health, there has been a pandemic-related increase in oral health risk factors.10 The present study was undertaken to evaluate the impact of the COVID-19 pandemic on childrens’ oral health status and caregiver’s attitudes toward teledentistry in two cities. In the present study, the maximum caregivers were in the age group of 30–40 years and most of them were female. Out of 583 caregivers who participated in the study, 545 were not satisfied with their child’s oral health status, out of which 47% were male and 53% were female. Twenty-eight participants were satisfied with their child’s oral health, in which all were female. This suggests that none of the male participants were satisfied with their child’s oral health status during the pandemic. Also, out of 28 female participants who were satisfied with the oral health status of their children, the maximum were between 30 and 40 years of age and had a bachelor’s degree. According to a study from China19, 44.2% of caregivers of school-going age children were not satisfied with their children’s oral health status during the pandemic period and revealed that their children suffered from dental pain or discomfort during this period.
In the present study, approximately 91% of the caregivers agreed that COVID-19 pandemic has a negative effect on their child’s oral health, while approximately 9% of them did not agree. Around 34.3% of the caregivers think that alteration in sleep pattern is the reason that affected their child’s oral health during the pandemic, 32.9% of caregivers think that quarantine and social restriction is the cause, whereas according to 32.8% of caregivers, feeding style is the main cause that affected their child’s oral health. In a Brazilian study done in the year 2020, authors have observed that there was a change in day-to-day eating habits and routine in most families during the COVID-19 pandemic. Around 61.5% of the participants revealed changes in feeding patterns during the pandemic and most of them reported an increase in food intake, out of which approximately 67% admitted consuming processed foods and snacks. It was also found that there was a remarkable impact of COVID-19 on caregivers’ attitudes towards seeking dental care for their children during this pandemic situation as most of them revealed that they would seek only emergency dental treatment.2
Dentistry requires close face-to-face contact with the patient. Due to this reason, dental clinics have been mostly suspended during the global pandemic situation. Only emergency care was permitted to reduce the risk of transmission of COVID-19 disease.20,21 According to studies reported in the literature, COVID-19 pandemic waves have tremendously affected routine dental care worldwide.22–30 It has also been reported that COVID-19 spreads through droplet contact.31 Since most dental procedures are known to produce an aerosol, there is always a risk of infection spread to the dental clinicians and others who are present in the dental studio.32 Thus, dental professionals have been kept in a very high exposure risk category by Occupational Safety and Health Administration.33 In addition to this, many people were frightened due to the risk of virus transmission and were not ready to visit the dental clinic for mild to moderate dental discomforts.34 Moreover, the extended period of absence of regular oral health checkups often results in periodontitis in many cases.35,36 The concept of teledentistry has largely grabbed attention and has emerged as a boon during this pandemic period to overcome the hindrance in seeking routine dental care for patients. Teledentistry is an amalgamation of telecommunication and dentistry, which allows sharing of clinical information and images for dental consultation and treatment planning.37 Thus, teledentistry offers an alternative solution to continue dental practice amidst this COVID-19 pandemic.
Although 544 caregivers have reported utilizing teledentistry during the pandemic in the present study, 310 of them were not sure if teledentistry can fulfill the oral healthcare needs of their children. Only one female caregiver, aged more than 40 years, totally agreed that teledentistry can be used to provide oral healthcare, while 232 caregivers agreed to some extent with the above statement. Rahman et al.38 evaluated patient response to teledentistry and they observed more than 96% patient satisfaction with telephonic consultation and virtual clinics. This study also suggested that teledentistry can be a promising solution to the oral healthcare needs of patients during a pandemic situation.
There are various subunits of teledentistry including teleconsultation, telediagnosis, patient electronic records, patient referral, teletriage, and telemonitoring pertinent to dental practice.39,40,41 In the present study, most of the caregivers (38.6%) reported that telediagnosis is the most useful subunit of teledentistry for children. Being a recent concept, teledentistry faces acceptance challenges among clinicians as well as patients in terms of security, patient privacy, and other issues.42 Numerous opinions and conclusions have been given by various authors around the globe.43–56 However, the majority of them addressed that teledentistry has become popular during the pandemic period.50–57 It is important to emphasize the benefits of teledentistry among dentists and to increase awareness about it among health care professionals and the general population.58-60
Limitations of the study
Data assessed in the study solely depend on the caregiver’s report and retrospective anamnesis, which is a limitation of the study. Since this study was an online survey, people who didn’t have knowledge and access to the Internet could not participate in the study.
CONCLUSION
COVID-19 has affected almost every segment of society from infants to elderly people in some way. The present study concludes that COVID-19 pandemic has a negative impact on the oral health of children and the caregivers of these children are not well aware of the benefits of teledentistry. Teledentistry can be useful during a challenging pandemic situation and hence it is recommended to increase awareness about the uses and advantages of teledentistry among the population of Kuwait.