INTRODUCTION
A new type of coronavirus family SARS-CoV-2 has been detected in individuals with several clinical symptoms. This virus was discovered in late 2019 in Wuhan, China, and it was named COVID-19. This virus has spread throughout the whole world rapidly, and was recognized as a pandemic on March 11, 2020.1 There are many researches about the cutaneous findings related to COVID-19.2 Numerous researches have been conducted on the manifestations of skin problems related to COVID-19, i.e. rashes, Pityriasis rosea (PR), vascular markings or pimple like lesions.3 PR is a papulosquamous trouble, first described by Robert Willan in 1798, but under a different terminology.4 PR is described as a skin eruption with initial popping spots, followed by division dermatose lines appearing as minimal, separate, oval to round lesions of skin on collarbone area. Such lesions are chiefly found on proximal and trunk sides. A spontaneous remission typically takes place during the rash’s appearance of 6-12 weeks. PR is thought to be associated with viral infections, particularly human herpes virus (HHV) 7.5 There were many names for PR initially, but it was later named Herpes maculosus and Roseola annulet.6 It typically appears first as a huge erythematous scaly plaque evolution, which is termed as mother patch or herald patch, on neck or trunk. It is then followed by multiple secondary tiny erythematous scaly lesions or rashes predominantly located on the trunk, and followed by split lines on the back.7
Since coronavirus is closely related to PR, and we can predict the infection from the beginning, as it is considered an early diagnostic sign. However, there is no evidence that coronavirus is the cause of PR, due to different types of rashes that appear on the infected area.8 It is very common. The incidence of PR was 0.39 to 4.8 per 100 dermatology patients.5 The etiology of PR is unknown, and the lesions’ histopathological alterations are non-specific for PR. They contain focal spongiosis caps, vascular dilation, infiltrates are perivascular lymphocytic, and parakeratosis are patchy. These cytological changes are close to viral infections, i.e., varicella zoster and herpes simplex.9 The goal of the current work is to observe if coronavirus is a risky factor in PR development, where it might be considered as a trigger for other types of infection, including PR. It can be considered a symptom of infection with the virus.
MATERIAL AND METHODS
This study is a case series describing the dermatological findings related COVID-19 in Thi-Qar Governorate, Iraq. The samples for this study were gathered from inpatients, outpatients, and emergency units of Al Hussein Teaching Hospital, and the inwards of Al-Shefaa’ Isolation Hospital. The study was conducted over a four-month period, i.e., from June to September, 2020. A total of 19 patients, 10 females and 9 males were included in the study. All cases were proved to be COVID-19 positive by post nasal or pharyngeal swab for PCR technique. A verbal consent was taken from each patient with a full description of the aim and benefit of the study. A skin lesion was first identified by a dermatologist. Skin scraps were taken from the lesion of those who were infected with COVID-19 and diagnosed with histo-pathological changes. Even though they were non-specific for PR, they were highly suggestive. Most of the lesions contain focal spongiosis caps, vascular dilation, infiltrates as perivascular lymphocytic, and parakeratosis as patchy. The samples were classified by internist into mild, moderate, and severe cases of COVID-19 according to WHO criteria, and they were also categorized as typical and atypical according to PR. Statistical analysis was done using SPSS version. There were 26 describing cases according to their presentation regarding their mean age, gender, severity of COVID-19 and sub-types of (PR). ANOVA and Fischer Exact Tests were used for cross-tabling to study the association of the variables of interest, and P value <0.05 was of great significance.
RESULTS
Nineteen patients in total (10 females, 9 males), who were infected with COVID-19 and were suffering from PR were included in this study, of which 52.6% were female and 47.4% were male (Figure 1).
FIGURE 1. Distribution according to gender.

FIGURE 2. Distribution according to PR sub-types

FIGURE 3. Distribution according to COVID-19 sub-category
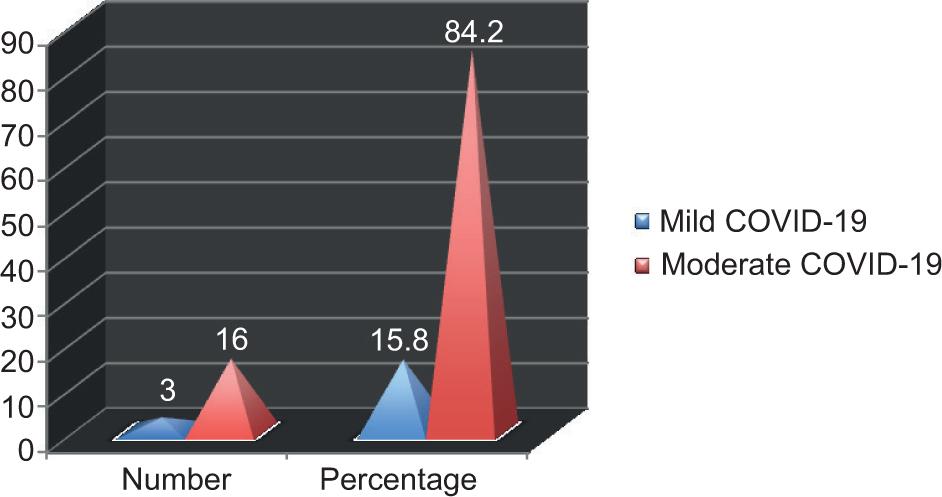
FIGURE 4. Different presentations of PR.

Figure two demonstrates the distribution of patients according to the incidence of PR in typical and anomalous manner. The highest percentage was 77.9% for typical and 21.1% for abnormal.
A distribution of infected people were observed according to the COVID-19 sub-category. The highest percentage was of moderate COVID-19 i.e., 84.2%, while in mild COVID-19 it was 15.8%.
Table 1 refers to the mean age distribution according to gender, in which there is no significant statistical difference, while a higher statistical difference can be seen in PR and COVID-19 categories.
TABLE 1. Mean age distribution according to gender, skin lesion and severity of COVID-19
| Variables of interest | Mean | Standard Deviation | ANOVA, p-value, Eta |
|---|---|---|---|
| Sex | .547 | ||
| Male | 26.2222 | 4.54911 | .470 |
| Female | 28.0000 | 5.77350 | .177 |
| P. Rosea | |||
| Typical | 28.1333 | 5.26263 | 2.792,0.113 |
| Atypical | 23.5000 | 2.88675 | .376 |
| COVID-19 severity | |||
| Mild | 27.0000 | 5.60952 | .090, 0.768 |
| Moderate | 28.0000 | 1.73205 | 0.073 |
| Total | 27.1579 | 5.16681 | |
TABLE 2. The distribution of patients with PR according to their gender and the severity of COVID-19
| Sex | Sex | Fischer Exact | |||||
|---|---|---|---|---|---|---|---|
| Mild | Moderate | Total | |||||
| Male | PR | Typical | No. | 5 | 2 | 7 | .735e |
| % | 71.4% | 28.6% | 100.0% | ||||
| Atypical | No. | 2 | 0 | 2 | |||
| % | 100.0% | 0.0% | 100.0% | ||||
| Total | No. | 7 | 2 | 9 | |||
| % | 77.8% | 22.2% | 100.0% | ||||
| Female | PR | Typical | No. | 8 | 0 | 8 | 4.444 |
| % | 100.0% | 0.0% | 100.0% | ||||
| Atypical | No. | 1 | 1 | 2 | |||
| % | 50.0% | 50.0% | 100.0% | ||||
| Total | No. | 9 | 1 | 10 | |||
| % | 90.0% | 10.0% | 100.0% | ||||
| Total | PR | Typical | No. | 13 | 2 | 15 | |
| % | 86.7% | 13.3% | 100.0% | ||||
| Atypical | No. | 3 | 1 | 4 | |||
| % | 75.0% | 25.0% | 100.0% | ||||
| Total | No. | 16 | 3 | 19 | |||
| % | 84.2% | 15.8% | 100.0% | ||||
There are no significant statistical differences in the gender distribution for the subtypes of COVID-19 according to pit. Rosea subclass.
DISCUSSION
COVID-19 has had several influences on the dermatology that have been practiced routinely.10 It is obvious that we would witness developments in this field, and more accurate data would be collected about the relation between dermatology and COVID-19 in the coming days. Cutaneous symptoms can be classified under five chief groups: livedo and necrosis, lesions as urticarial, eruption being maculopapular, pseudo-chilblain, and rash as vesicular.2 At present, the skin diseases which accompany people with COVID-19 remain an unresolved mystery. In the current research, it was observed that the average PR patients, who have applied to outpatient dermatology clinic throughout the period of the pandemic, has increased multiple times in the current year, as compared with same time last year. PR has been highly linked with people with Herpes Virus 6 and 7 reactivation, while other etiology such as viral fever, stress being psychological, vaccination, and drugs as the reaction cause.11 In many sources, it may be one of the factors leading to the activation of herpes viruses in which corona viruses can be the cause of PR. Or perhaps, stress and psychological pressure caused by the period of the epidemic being another cause.12
In the previous study, it was shown that the rashes and skin diseases associated with those who were infected with COVID-19 differed dramatically according to the geographical location.13 In the previous research conducted by Enguix et al., when people with PR performed a COVID-19 test using PCR, a positive result was obtained which is consistent with the current study. COVID-19 influences multiple organ systems to uncontrolled release of pro-inflammatory chemokines and cytokines, causing the manifestation of clinically excluding symptoms of respiratory system.15 This is the first study in Thi-Qar, Iraq, that that shows PR throughout the period of the pandemic. We believe that such elevation is associated with HHV-6 reactivation. It is possible that PR is a symptom of the COVID-19. This disease still remains as an unresolved mystery. However, there are numerous published articles about the clinical symptoms and side effects. More studies are needed based on the antibody polymerase and PCR, which should be implemented to search if there are any specific dermatologic diseases are connected to the cases of asymptomatic COVID-19.16 There are no adequate studies so far in order to enable clinicians to recognize definite patterns of skin problems relating to COVID-19. Therefore, it is important to state these cases in order to increase the knowledge regarding such symptoms, particularly because they can be the only infection signs, and can be confused with other viral infection and skin diseases. We also presume the importance of distinguishing between different mechanisms like physiological and temporal patterns to understand whether there is a viral synergistic or symbiotic relationship with other processes such as erythema, infection, herpes zoster, and other skin diseases. Moreover, we highlight the importance of screening the precarious skin diseases in patients infected with COVID-19. More studies are needed to evaluate whether or not these lesions are associated with the virus. More accurate cutaneous manifestation of COVID-19 is required to increase the presentation of these diseases as well as epidemiological knowledge.
In a previous study conducted by Haha, it has been shown that being infected with PR has no relationship to people with Coronavirus. It is imperative for all healthcare professionals to be well-versed in such elevated manifestations of COVID-19. Surgeons should be also aware of such lesions, as they appear on feet, hands, and torso often. Further, COVID-19 standardized studies of rash are warranted for additional valid diagnosis and such visible endings utility.17
PR infection increased during the COVID-19 outbreak. This increase may be related to intense stress during the pandemic period, or as a marker in COVID-19 patients. It is possible that altered immunity during the COVID-19 pandemic increased the frequency of PR infection. Moreover, we should keep in mind that PR infection may be accompanied by COVID-19.
One limitation of the current work was the incapability of collecting standardized and complete sets of data to permit comparisons in depth among sub-groups of rash. In a previous study conducted by Catala et al., it showed that the infection with PR was related to the Coronavirus, as the percentage of patients with PR reached 30%. In conclusion, a description of PR related to COVID-19 might help doctors approaching patients who have such disease and recognizing cases of little symptoms. Ehsani et al. reported PR in a patient with COVID-19. A scaly annular rash over arms and trunk was observed in the 27 year-old-man. The lesions were pruritic and spread over five days.19 But, another study Mawhirt et al. confirmed that there is no relationship between COVID-19 and skin infections such as PR. The reason for the appearance of PR spots might be just the activation of a specific virus relating to retrospective work. There was no information about the individual’s quality of life, levels of anxiety, their treatments, and the risk of COVID-19. The current work is trying to understand the reason why patients with minor dermatological diseases visit hospitals, while a worldwide fatal pandemic is occurring at the same time.21 The rash of PR may be a direct result of virus-organ interaction, or the result of an immune system activation.22 It is necessary to emphasize such patterns for clinical diagnosis. Furthermore, we suggest that researches should be enriched by conducting extra COVID-19 tests for diagnoses, as well as describing some collected markers and the clinical link between them.23,24
CONCLUSION
PR is one of dermatological findings related to COVID-19 that does not have a clear role in its distribution according to the biography of the patient. It has not distributed significantly according to the severity of COVID-19. It might be triggered by COVID-19 and be completely cured with the clearance of disease.
RECOMMENDATION
More accurate cutaneous documentation of COVID-19 is required to increase the presentation of these diseases as well as epidemiological knowledge.