
FIG 1. Postoperative anteroposterior (A) and lateral (B) radiographs showed knee replacement loosening at 12-month follow-up.
Case Report
Hassan Zmerly1,2, Manuela Moscato1, Vincenzo Mancuso3 and Valentina Di Gregori1
1GVM Care and Research, S. Pier Damiano Hospital, Faenza, RA, Italy
2UCM Malta, Ludes Campus, Lugano, Switzerland
3Azienda ASL, Imola, BO, Italy
Hypersensitivity to implant components and periprosthetic joint infection should be detected before all revision arthroplasty, as misdiagnosis can lead to replacement loosening and the need for further revision procedures. We describe the case of a 69-year-old woman presenting a history of a painful cemented total knee replacement. Postoperative investigations showed loosening of X-ray components, suspected periprosthetic joint infection, and patch test hypersensitivity to nickel sulfate and methyl methacrylate. Two months later, a more specific patch test indicated non-allergy to the solid scratch of one bone cement. The patient underwent a two-stage revision with prosthesis removal and the temporary application of a specific cement spacer followed by the successful reimplantation of a cemented revision prosthesis. All candidates for the revision arthroplasty procedure must be investigated for hypersensitivity to metal and bone cement in order to avoid complications related to prosthesis intolerance and the need for further revision surgery; in the presence of hypersensitivity to bone cement and periprosthetic joint infection with a two-stage revision indication, the patient must be submitted to further patch tests with scratches of solid bone cement.
Keywords: allergy; metal; bone cement; periprosthetic joint infection; revision total knee arthroplasty
Total knee arthroplasty (TKA) is one of the most common surgical procedures in elective orthopedic surgery, with the number of procedures rising because of the increasing age of the population.1 Arthroplasty revision represents a major problem in the case of a painful joint prosthesis, some investigations are necessary to detect the origin of the symptomatology.1–3
Infection, malalignment, instability, and patellar pain are the principal reasons for a revision procedure; but, in rare cases, implant component hypersensitivity can occur, resulting in the replacement failure.4–6
Even when the failure is because of the mechanical etiology, a periprosthetic joint infection and component hypersensitivity must be excluded before the revision procedure. In the case of metal hypersensitivity, a non-allergic prosthesis must be used, while, in the case of infection, a two-stage revision is indicated with the temporary use of a cement spacer. In a patient with bone cement hypersensitivity, the choice is between a primary or a revision cementless prosthesis, but the cement spacer is contraindicated.7 In this report, we describe the case of TKA loosening in which postoperative diagnostic tests revealed nickel sulfate and methyl methacrylate hypersensitivity, with suspected periprosthetic joint infection.
With the consent of the patient, we report the case of a 69-year-old woman with knee osteoarthritis (OA) who was admitted to our department. She presented with a medical history of left knee pain, swelling and giving way, with progressive activity limitation for the past 5 years. Three years ago, she had undergone an arthroscopic joint debridement, but this resulted in a poor outcome. Weight-bearing radiography showed severe OA in the left knee with a significantly reduced joint space. The patient consented to TKA of the left knee. No history of allergy was reported. A cemented mobile-bearing TKA was performed. No complications or adverse events occurred during the surgery. After a regular postoperative period of 6 months, the patient experienced pain, swelling, erythema, and hyperthermia in the operated knee with a progressive loss of motion. She also reported recurrent episodes of skin pruritus on her thigh and the operated knee. At 8 to 12 months after surgery, some investigations were conducted: an X-ray showed tibial and femoral loosening (Figure 1). The laboratory tests revealed the following: white blood cell count=8,700/μL, eosinophils=6.6% (normal value=1–6%), erythrocyte sedimentation rate=49 mm/h (normal value<20 mm/h), and C-reactive protein (CRP)=3.2 mg/dL (normal<0.50 mg/dL). Further, synovial fluid aspiration chemical analysis was not significant, while a culture examination was negative for microbiological growth. A leukocytes isotope scan revealed an uptake on the femoral and tibial side. Two patch tests were performed by different allergy centers, showing a positive allergic reaction to nickel sulfate and methyl methacrylate.

FIG 1. Postoperative anteroposterior (A) and lateral (B) radiographs showed knee replacement loosening at 12-month follow-up.
The patient was a candidate for a two-stage revision with prosthesis removal and the temporary application of a cement spacer; however, the allergy contraindicated the use of bone cement. Two months later, two further patch tests with scratches of solid bone cement were conducted, and the allergist suggested the use of bone cement which did not produce any allergic reaction at 3–5 days.
During the removal of the implant, several samples from different knee localizations were collected for histopathological and microbiological examinations. The prosthesis sonification technique was also applied. All investigations showed the absence of infection.
With the cement spacer (Figure 2), the patient was able to walk with two crutches and a brace; no dermatologic or other allergic reactions occurred. The revision non-allergic cemented prosthesis procedure (Oxinium) femoral component and nickel-free tibial component was performed 13 weeks after primary prosthesis removal. At 10-month follow-up, the patient was free of symptoms with a good X-ray outcome (Figure 3). Negative blood analysis results, for example, regarding eosinophils (4.6%, normal value=1–6%) and CRP (3.7 mg/dL, normal value <0.50), were returned after surgical treatment.

FIG 2. Anteroposterior radiograph after prosthesis removal and cement spacer implant.
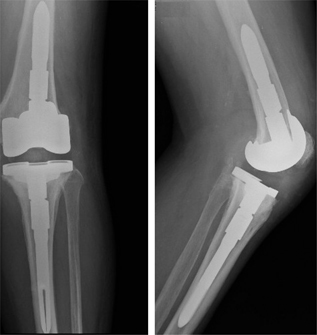
FIG 3. Radiographic anteroposterior (A) and lateral (B) showed good outcome of revision total knee arthroplasty at 10-month follow-up.
The amount of revision arthroplasty procedures is estimated to rise due to the high number of primary TKA interventions performed every year globally. In the case of aseptic loosening, a one-stage revision can be performed but, if periprosthetic joint infection is present, a two-stage revision is recommended; further, before all revision procedures, infection must be excluded and an allergic evaluation must be conducted.8,9
The management of joint periprosthetic infection is a challenge, and the diagnosis must include the following: knee examination, accurate history, blood test, knee aspiration, imaging (including radiographs), ultrasound assessment, leukocytes isotope scan, and histological polymorphonuclear leukocyte count.
Detecting allergy to an arthroplasty component is of vital importance, because misdiagnosis can lead to implant loosening with the need for a non-allergic substitution of the prosthesis.8 Hypersensitivity to prosthesis implant materials and bone cement is rare, but all patients with a history of suspected allergy who are candidates for primary or revision arthroplasty should be assessed using a patch test for allergy to all of the implant components prior to the surgical procedure, as misdiagnosis can lead to implant failure. The gold-standard diagnostic method for the confirmation of an allergy is the skin patch test.10,11
The post-arthroplasty finding of metal and bone cement hypersensitivity with joint periprosthetic infection is an exceptionally rare event. To the best of our knowledge, this is the first case described in the English-language medical literature. In patients with an allergy to nickel and bone cement who need a one-stage revision, it is possible to use cementless non-allergic primary or revision prosthesis based on the amount of bone stock and the ligaments’ stability; however, in the case of periprosthetic joint infection, the treatment of choice is a two-stage revision, where, in the first step, the prosthesis must be removed and replaced with a cement spacer. But, when hypersensitivity to bone cement is present, the use of a cement spacer is contraindicated and there is no effective alternative solution available.12–14
Stathopoulos15 described the case of a patient who underwent knee arthroplasty and developed pain and an allergic reaction due to hypersensitivity to metal and bone cement without signs of infection. The patient was treated successfully with the removal of the implant and a one-stage revision with a hypoallergenic cemented prosthesis. In our patient, based on the clinical examination, history, blood test, and leukocytes isotope scan, we performed a two-stage revision because it was not possible to exclude a low-aggressive infection.
Despite positive patch tests for hypersensitivity to nickel and methyl methacrylate, fortunately, further patch tests with scratches of bone cement produced negative results; the use of a temporary cement spacer confirms non-reactivity against the type of bone cement used. Our study adds an atypical pattern of patient allergies to the findings on sensitization to cement, even though the allergy was not retrieved. The limitation of the present study is the possibility of false-positive as well as false-negative results.
The histopathological and microbiological examinations with prosthesis sonification showed the absence of infection and the two-stage procedure may not have been necessary; but it helped us to confirm the non-allergy against the type of cement chosen.
In patients who have undergone TKA, the postoperative finding of metal and methyl methacrylate hypersensitivity in the presence of periprosthetic joint infection is an exceptionally rare but nevertheless a devastating event; in such a situation the patient will be submitted to further investigations including a patch test for scratches of solid bone cement.